TRAUMA-
Women and PTSD: Using a Trauma-Informed Approach to Heal.
How to build a safe and soothing environment to recover from past traumas.
Reviewed by Ekua Hagan
KEY POINTS-
Untreated trauma can lead to PTSD, which females experience at nearly twice the rate as their male counterparts.
A recent CDC study reveals a sharp rise in sexual violence and attempted suicide rates among teen girls.
While EMDR is not a one-size-fits-all treatment, it has been found to be helpful in treating a variety of traumatic experiences.
A recent CDC study revealed that from 2017 to 2021, the number of teen girls in the United States who experienced sexual violence increased by 20 percent. On top of that, the study also shows in 2021, nearly 1 in 3 teen girls seriously considered attempting suicide.
Experiencing something traumatic, such as sexual abuse or violence, increases your risk of developing post-traumatic stress disorder (PTSD) in the future. The concerning and disheartening results of the CDC study serve as an alarm for healthcare providers everywhere to be equipped to handle an influx of young females who may be desperately trying to heal from serious mental health struggles. To start, we should look at how we define trauma and how it may lead to PTSD.
What Is Trauma?
When you hear the word “trauma,” what comes to mind? Perhaps a natural disaster, poverty, prolonged neglect, violence, or abuse? Trauma, by definition, is a lasting emotional response to intensely distressing events or situations that occur when we fall outside of our ability to cope. Everyone's experience of trauma can be subjective and unique, which is why a divorce, for instance, can be experienced as traumatic for one person but not another.
At the time of a traumatic event, the strong emotions you experience can interfere with your ability to completely process the event, and this one unpleasant moment becomes “frozen in time.” Eventually, if not addressed, you may develop post-traumatic stress disorder, a mental health condition that is triggered by an overwhelming event—either experiencing it or witnessing it. Some of the most common PTSD symptoms include flashbacks, nightmares, and severe anxiety, as well as uncontrollable thoughts about the event, avoidance, and substance misuse. While this condition is certainly a possibility, it is important to note that not all people who experience a traumatic event will go on to develop PTSD.
When receiving a diagnosis, it is easy to feel as though there is something wrong with us, but keep in mind that our bodies and brains are engaging in completely normal survival responses to abnormal circumstances. Therefore, many practitioners will refer to this experience as post-traumatic stress injury, rather than a disorder.
Are Women at Risk of Experiencing More Trauma?
Research suggests that people of all gender identifications can experience trauma, so it is important for healthcare professionals to approach the topic without gender bias. However, statistics show that women may be more likely to experience certain types of traumatic events, such as physical and sexual violence by intimate partners. For transgender and non-conforming individuals, the rates tend to be even higher.
The National Center for Victims of Crime reports that 1 in 5 women in the United States has experienced rape or attempted rape in her lifetime. Sexual assault is often underreported, and even within relationships, forced intimacy without consent or consent while under the influence can be considered assault.
When it comes to the effects of trauma, studies have shown that women's brains may respond differently than men's. Women can have higher rates of reexperiencing events, negative alterations in cognition or mood, and dissociative responses, among other post-traumatic reactions. Something else worth noting is that women typically have different ways of expressing their emotions compared to men, with women more likely to use words such as "anxiety.” Therapeutic providers must take these gender-specific differences into account when providing care for their clients.
Over time, some individuals learn how to cope with their trauma in healthy ways, however, there are many female survivors who cannot fully process the event and/or are afraid to reach out for help. As mentioned earlier, untreated trauma can lead to PTSD, which females experience at nearly twice the rate as their male counterparts. Aside from mental health consequences, those living with unresolved trauma may also struggle with physical side effects like gastrointestinal issues and sexual dysfunction.
Emotional Distress and Trauma in Young Women
Uncovering why women tend to experience more trauma than men is a complex issue with many layers. In looking at the previous CDC study, we can see in 2021, 3 in 5 young women in their early teens were feeling persistently sad and hopeless, common precursors to depression. These are the highest levels of sadness and hopelessness seen in a decade and nearly twice the rate among teenage boys. This trend is also reflected in members of the LGBTQ+ community with 55 percent of young teens experiencing poor mental health.
While emotional distress does not necessarily correlate with trauma in young girls, we, as healthcare providers, need to stay attuned to what this trend can potentially manifest into. Teen girls struggling with these strong feelings may pull away from their loved ones and lose interest in their favorite hobbies and activities. To distract from feelings of low self-esteem, teens may experiment with substances, make impulsive decisions and, at times, engage in higher-risk sexual activity.
The CDC study also shared that since 2019, young females being forced to have sex has increased by 27 percent. Traumatic experiences such as this can be very harmful to a teenager's emotional development, therefore, it is important for survivors to fully process the memory and move forward in a meaningful way. Teens struggling with a traumatic incident might have trouble forming healthy relationships due to a lack of trust and poor boundary observance as well as increased behavioral issues and emotional dysregulation.
Rather than seeing these statistics as an indication of something "wrong" with those who identify as female and non-conforming individuals, we must focus on how to support them and create a more resilient and uplifting environment. This can involve providing resources and tools for managing difficult emotions and experiences, like support groups and systematic trauma screening. Recognizing the strengths of women who have experienced trauma, such as their courage and resourcefulness in coping with difficult situations, can help them build upon their existing strengths and develop new ones. If we focus on recovery, rather than pathology, we can create a more positive and empowering narrative around mental health and trauma.
What Does a Trauma-Informed Treatment Approach Look Like?
Although we have a considerable amount of knowledge about how trauma and PTSD impact an individual, how we respond as care providers is crucial to the healing process for those with whom we work.
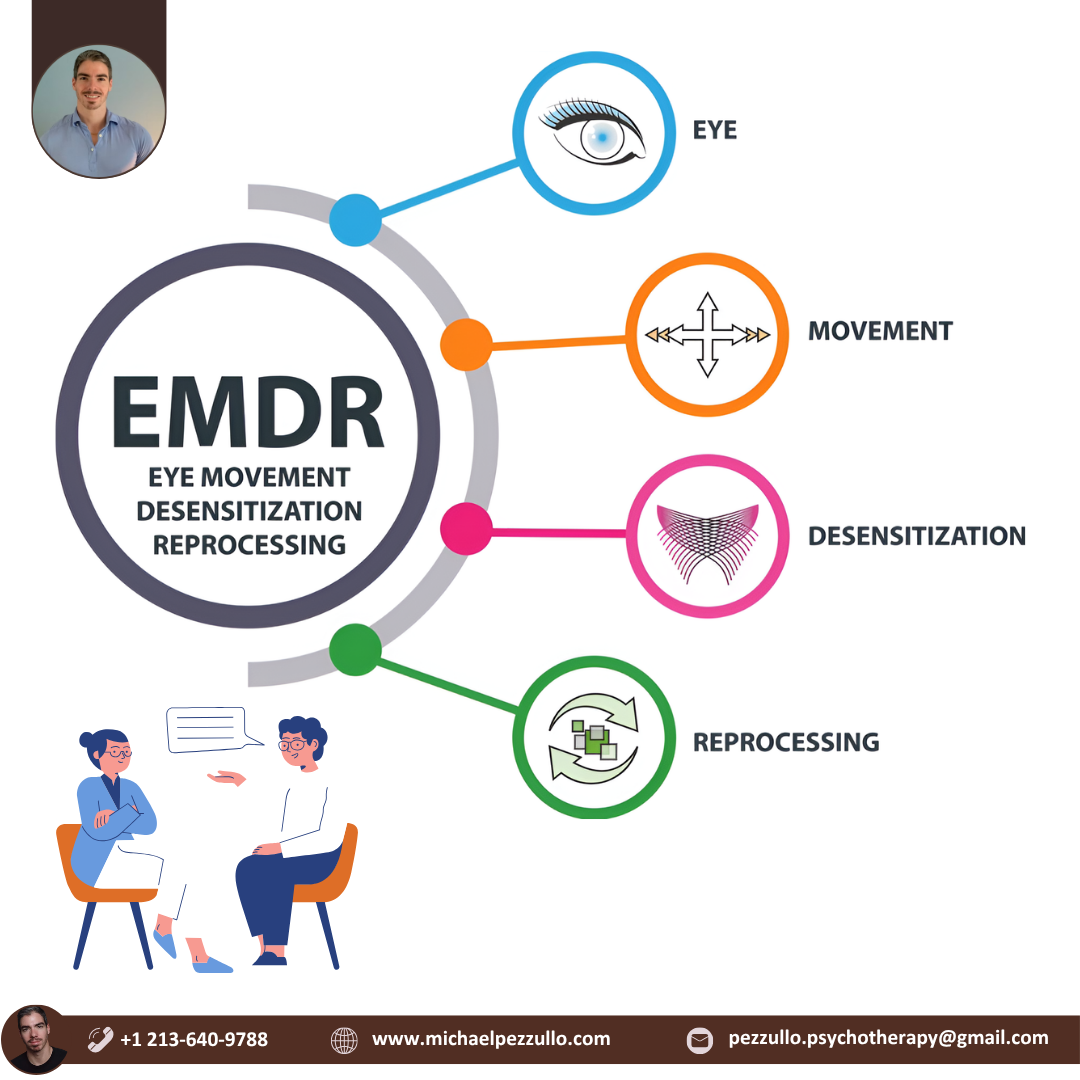
A trauma-informed treatment approach looks at an individual's experiences and past traumas to better understand and address their current physical and emotional challenges. This approach prioritizes creating a safe and supportive therapeutic environment where the client feels comfortable to share openly. Clinicians might use somatic therapies, such as Eye Movement Desensitization and Reprocessing (EMDR), which recognize that trauma can be stored in the body and can manifest in behavioral disorders and compulsions like eating disorders and substance use disorders. EMDR is an evidence-based psychotherapy that helps individuals reprocess traumatic memories to heal from PTSD.
One meta-analysis of 23 studies found that EMDR was effective in reducing symptoms of PTSD, depression, and anxiety. While EMDR is not a one-size-fits-all treatment and may not be effective for everyone, it has been found to be helpful in treating a variety of traumatic experiences, from combat and sexual assault to natural disasters, accidents, and childhood abuse.
By acknowledging the connection between the body and trauma, EMDR allows the individual to utilize their body's natural healing processes in the therapeutic journey. EMDR's client-centered approach puts the client in the driver's seat, empowering them to take an active role in their healing. Overall, EMDR provides a unique and effective pathway for women to address past traumas and move towards a more fulfilling future.
Although many women may deal with trauma and PTSD throughout their lifetimes, healing is possible. To help survivors navigate their struggles, we must provide more resources such as peer support groups, education on consent and healthy relationships, and accessible treatment options.
If you or someone you love is contemplating suicide, seek help immediately. For help 24/7 contact the National Suicide Prevention Lifeline, 1-800-273-TALK, or the Crisis Text Line by texting TALK to 741741.
TRAUMA-
Women and PTSD: Using a Trauma-Informed Approach to Heal.
How to build a safe and soothing environment to recover from past traumas.
Reviewed by Ekua Hagan
KEY POINTS-
Untreated trauma can lead to PTSD, which females experience at nearly twice the rate as their male counterparts.
A recent CDC study reveals a sharp rise in sexual violence and attempted suicide rates among teen girls.
While EMDR is not a one-size-fits-all treatment, it has been found to be helpful in treating a variety of traumatic experiences.
A recent CDC study revealed that from 2017 to 2021, the number of teen girls in the United States who experienced sexual violence increased by 20 percent. On top of that, the study also shows in 2021, nearly 1 in 3 teen girls seriously considered attempting suicide.
Experiencing something traumatic, such as sexual abuse or violence, increases your risk of developing post-traumatic stress disorder (PTSD) in the future. The concerning and disheartening results of the CDC study serve as an alarm for healthcare providers everywhere to be equipped to handle an influx of young females who may be desperately trying to heal from serious mental health struggles. To start, we should look at how we define trauma and how it may lead to PTSD.
What Is Trauma?
When you hear the word “trauma,” what comes to mind? Perhaps a natural disaster, poverty, prolonged neglect, violence, or abuse? Trauma, by definition, is a lasting emotional response to intensely distressing events or situations that occur when we fall outside of our ability to cope. Everyone's experience of trauma can be subjective and unique, which is why a divorce, for instance, can be experienced as traumatic for one person but not another.
At the time of a traumatic event, the strong emotions you experience can interfere with your ability to completely process the event, and this one unpleasant moment becomes “frozen in time.” Eventually, if not addressed, you may develop post-traumatic stress disorder, a mental health condition that is triggered by an overwhelming event—either experiencing it or witnessing it. Some of the most common PTSD symptoms include flashbacks, nightmares, and severe anxiety, as well as uncontrollable thoughts about the event, avoidance, and substance misuse. While this condition is certainly a possibility, it is important to note that not all people who experience a traumatic event will go on to develop PTSD.
When receiving a diagnosis, it is easy to feel as though there is something wrong with us, but keep in mind that our bodies and brains are engaging in completely normal survival responses to abnormal circumstances. Therefore, many practitioners will refer to this experience as post-traumatic stress injury, rather than a disorder.
Are Women at Risk of Experiencing More Trauma?
Research suggests that people of all gender identifications can experience trauma, so it is important for healthcare professionals to approach the topic without gender bias. However, statistics show that women may be more likely to experience certain types of traumatic events, such as physical and sexual violence by intimate partners. For transgender and non-conforming individuals, the rates tend to be even higher.
The National Center for Victims of Crime reports that 1 in 5 women in the United States has experienced rape or attempted rape in her lifetime. Sexual assault is often underreported, and even within relationships, forced intimacy without consent or consent while under the influence can be considered assault.
When it comes to the effects of trauma, studies have shown that women's brains may respond differently than men's. Women can have higher rates of reexperiencing events, negative alterations in cognition or mood, and dissociative responses, among other post-traumatic reactions. Something else worth noting is that women typically have different ways of expressing their emotions compared to men, with women more likely to use words such as "anxiety.” Therapeutic providers must take these gender-specific differences into account when providing care for their clients.
Over time, some individuals learn how to cope with their trauma in healthy ways, however, there are many female survivors who cannot fully process the event and/or are afraid to reach out for help. As mentioned earlier, untreated trauma can lead to PTSD, which females experience at nearly twice the rate as their male counterparts. Aside from mental health consequences, those living with unresolved trauma may also struggle with physical side effects like gastrointestinal issues and sexual dysfunction.
Emotional Distress and Trauma in Young Women
Uncovering why women tend to experience more trauma than men is a complex issue with many layers. In looking at the previous CDC study, we can see in 2021, 3 in 5 young women in their early teens were feeling persistently sad and hopeless, common precursors to depression. These are the highest levels of sadness and hopelessness seen in a decade and nearly twice the rate among teenage boys. This trend is also reflected in members of the LGBTQ+ community with 55 percent of young teens experiencing poor mental health.
While emotional distress does not necessarily correlate with trauma in young girls, we, as healthcare providers, need to stay attuned to what this trend can potentially manifest into. Teen girls struggling with these strong feelings may pull away from their loved ones and lose interest in their favorite hobbies and activities. To distract from feelings of low self-esteem, teens may experiment with substances, make impulsive decisions and, at times, engage in higher-risk sexual activity.
The CDC study also shared that since 2019, young females being forced to have sex has increased by 27 percent. Traumatic experiences such as this can be very harmful to a teenager's emotional development, therefore, it is important for survivors to fully process the memory and move forward in a meaningful way. Teens struggling with a traumatic incident might have trouble forming healthy relationships due to a lack of trust and poor boundary observance as well as increased behavioral issues and emotional dysregulation.
Rather than seeing these statistics as an indication of something "wrong" with those who identify as female and non-conforming individuals, we must focus on how to support them and create a more resilient and uplifting environment. This can involve providing resources and tools for managing difficult emotions and experiences, like support groups and systematic trauma screening. Recognizing the strengths of women who have experienced trauma, such as their courage and resourcefulness in coping with difficult situations, can help them build upon their existing strengths and develop new ones. If we focus on recovery, rather than pathology, we can create a more positive and empowering narrative around mental health and trauma.
What Does a Trauma-Informed Treatment Approach Look Like?
Although we have a considerable amount of knowledge about how trauma and PTSD impact an individual, how we respond as care providers is crucial to the healing process for those with whom we work.
A trauma-informed treatment approach looks at an individual's experiences and past traumas to better understand and address their current physical and emotional challenges. This approach prioritizes creating a safe and supportive therapeutic environment where the client feels comfortable to share openly. Clinicians might use somatic therapies, such as Eye Movement Desensitization and Reprocessing (EMDR), which recognize that trauma can be stored in the body and can manifest in behavioral disorders and compulsions like eating disorders and substance use disorders. EMDR is an evidence-based psychotherapy that helps individuals reprocess traumatic memories to heal from PTSD.
One meta-analysis of 23 studies found that EMDR was effective in reducing symptoms of PTSD, depression, and anxiety. While EMDR is not a one-size-fits-all treatment and may not be effective for everyone, it has been found to be helpful in treating a variety of traumatic experiences, from combat and sexual assault to natural disasters, accidents, and childhood abuse.
By acknowledging the connection between the body and trauma, EMDR allows the individual to utilize their body's natural healing processes in the therapeutic journey. EMDR's client-centered approach puts the client in the driver's seat, empowering them to take an active role in their healing. Overall, EMDR provides a unique and effective pathway for women to address past traumas and move towards a more fulfilling future.
Although many women may deal with trauma and PTSD throughout their lifetimes, healing is possible. To help survivors navigate their struggles, we must provide more resources such as peer support groups, education on consent and healthy relationships, and accessible treatment options.
If you or someone you love is contemplating suicide, seek help immediately. For help 24/7 contact the National Suicide Prevention Lifeline, 1-800-273-TALK, or the Crisis Text Line by texting TALK to 741741.